Table of Contents
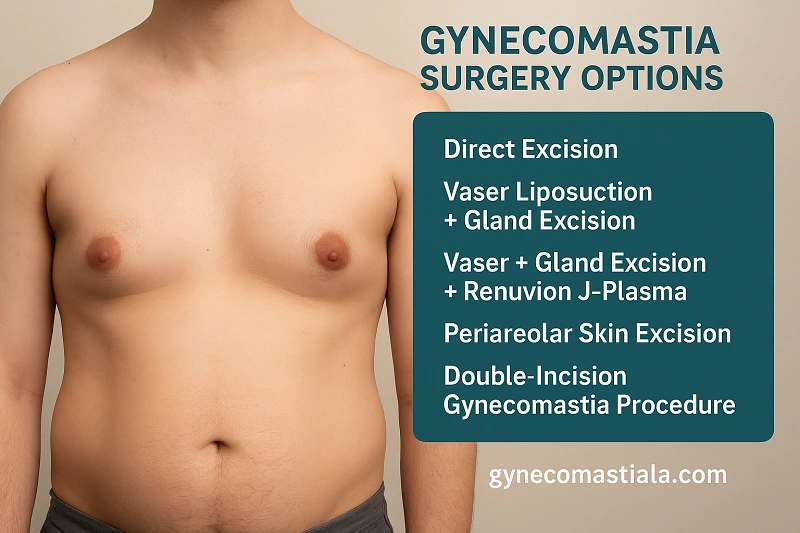
- Gynecomastia Surgery Techniques by Grade and Body Type
- 1. Direct Excision (Subareolar Excision)
- 2. Combined Vaser Liposuction + Gland Excision (Gold Standard)
- 3. Vaser + Gland Excision + Renuvion J-Plasma Skin Tightening
- 4. Periareolar Skin Excision with Combined Approach
- 5. Double-Incision Gynecomastia Procedure
- 6. Skin Resection + Gland Excision (Severe Cases)
- Choosing the Right Procedure: Decision Framework
- Risk-Benefit Analysis by Procedure
- Why Choose GynecomastiaLA in Los Angeles?
- Trust Your Results to Dr. Babak Moein in Los Angeles’ Distinguished Cosmetic Surgeon
Gynecomastia, the enlargement of male breast tissue, affects up to 65% of men at some point in their lives. Whether you’re a bodybuilder dealing with steroid-related tissue, a teenager with persistent pubertal gynecomastia, or an older gentleman experiencing age-related changes, understanding your surgical options is crucial for achieving optimal results.
This comprehensive guide will help you understand which procedure is most appropriate for your specific condition, grade of gynecomastia, and personal goals.
Gynecomastia Surgery Techniques by Grade and Body Type
Gynecomastia surgery is never a one-size-fits-all procedure. The most effective technique depends on both the grade of gynecomastia (I–IV) and the patient’s body type, skin quality, and aesthetic goals. In this section, we will review the main surgical options in detail and explain how each is selected. Drawing on the experience of Dr. Babak Moein, a leading dual board-certified general and cosmetic surgeon in Los Angeles, we will look at which technique is best suited for different grades of gynecomastia and for specific patient profiles, such as bodybuilders, teens, post-weight-loss patients, and men with severe skin laxity, so each patient can better understand which approach may be most appropriate for their case.
| Patient Type | Most Common Grade | Primary Procedure Choice | Key Consideration |
|---|---|---|---|
| Bodybuilders | Grade II | Combined VASER + Gland Excision | Preserve muscle definition; remove dense, steroid-induced glandular tissue. |
| Teens | Grade I–II | Direct Excision | Excellent skin elasticity; minimal scarring; ideally after hormonal stabilization (age 17–18). |
| Older Men | Grade II–III | VASER + Gland Excision ± Renuvion or Periareolar Excision | Address mixed tissue and mild laxity; medical optimization often required. |
| Overweight Men | Grade II–III | VASER + Gland Excision ± Renuvion | High-volume fat removal; consider preoperative weight optimization. |
| Puffy Nipples | Grade I | Direct Subareolar Excision | Localized gland removal with minimal access; restores flat contour. |
| Asymmetry | Variable | Customized Technique per Side | Individual surgical plan; realistic symmetry expectations are key. |
1. Direct Excision (Subareolar Excision)
What It Is: A time-tested surgical approach removing excess glandular tissue through a discreet incision along the lower areolar border.
Best Suited Gynecomastia Grades
Grade I: Localized gland under the areola with no skin excess (“puffy nipple”).
Grade II gynecomastia: with firm glandular tissue
Ideal Candidates for This Procedure
- Teenage Gynecomastia: Teen and young adult patients with a small, dense subareolar gland, tight skin, and a classic “puffy nipple” appearance.
- Bodybuilder Gynecomastia: Bodybuilders with steroid-related, firm glandular tissue under the areola and minimal surrounding fat who want precise gland removal without changing muscle shape.
- Revision Gynecomastia Surgery: Patients with residual glandular tissue after previous liposuction-only gynecomastia surgery who need targeted subareolar excision.
The Procedure: During surgery, a carefully placed semicircular incision follows the natural pigmentation border, allowing direct visualization and removal of the enlarged breast gland while preserving the nipple-areola complex and maintaining natural chest contour.
Benefits:
- Complete gland removal with direct visualization
- Well-camouflaged scar at areolar border
- Predictable results for fibrous tissue
- Excellent control over tissue excision
Considerations:
- Visible periareolar scar (though well-concealed)
- May require revision for fatty component
- Recovery time: 1-2 weeks for normal activities
2. Combined Vaser Liposuction + Gland Excision (Gold Standard)
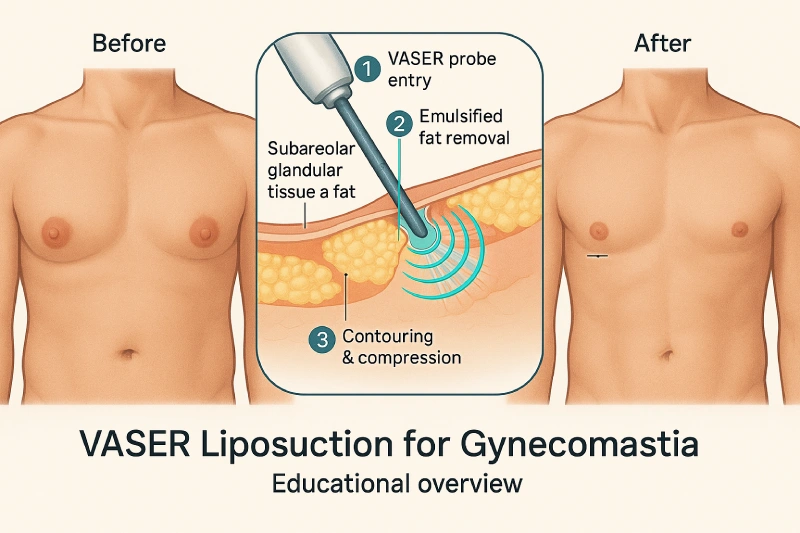
What It Is: The comprehensive approach combining ultrasound-assisted liposuction with direct glandular excision to address both fatty and glandular tissue components.
Best Suited Gynecomastia Grades


- Grade I–II: Mixed fat and glandular tissue with good skin elasticity.
- Selected Grade III: Moderate enlargement with mild skin laxity in patients who still have reasonable skin recoil.
Ideal Candidates for This Procedure
- Average-Weight Gynecomastia: Men at or near a healthy BMI who have a visible breast mound and fullness across the central and lateral chest.
- Overweight Gynecomastia: Men with mixed fat and glandular tissue (often BMI in the overweight range) who need both volume reduction and improved chest contour.
- Bodybuilder Gynecomastia: Muscular patients who require gland removal but also want high-definition contouring along the pectoral border and axillary roll.
- Lifestyle-Limited Gynecomastia: Men who avoid fitted shirts, swimming, or the gym because of chest projection but want to avoid larger skin-excision scars when their skin quality allows it.
The Procedure: High Definition Vaser technology emulsifies fat through ultrasonic energy, allowing smooth removal and enhanced pectoral muscle definition. After contouring the fatty layer, remaining fibrous glandular tissue is excised through a small periareolar incision.
Benefits:
- Addresses all tissue layers in single surgery
- Superior chest definition and contouring
- Enhanced skin retraction from Vaser energy
- Minimal incisions with excellent results
- Athletic, masculine chest appearance
Considerations:
- Higher cost than single-technique approaches
- Compression garment required for 4-6 weeks
- Temporary swelling and bruising
3. Vaser + Gland Excision + Renuvion J-Plasma Skin Tightening
What It Is: Triple-layer approach adding radiofrequency skin tightening for Grade III cases with mild skin laxity.
Best Suited Gynecomastia Grades
- Upper Grade II–Grade III: Extra tissue with mild to moderate skin laxity, but not enough to justify skin removal.
- Early Grade IV patients where skin is beginning to droop but can still retract with energy-based tightening.


Ideal Candidates for This Procedure
- Mild Skin-Laxity Gynecomastia: Men with moderate gland and fat who also show early sagging or softening of the lower chest but do not yet require formal skin excision.
- Post-Weight-Loss Gynecomastia: Patients after moderate weight loss who have loose skin and residual fullness but wish to avoid periareolar or double-incision scars if possible.
- Middle-Aged Gynecomastia: Men in their 30s to 50s with softer tissue quality and early ptosis who benefit from both tissue removal and energy-based skin tightening.
- Borderline Grade III–IV Gynecomastia: Patients on the edge between needing and not needing skin excision, where Renuvion J-Plasma may allow a tighter chest without larger incisions.
The Procedure: Combines Vaser liposuction and gland excision with Renuvion J-Plasma technology, which delivers controlled thermal energy subdermally to stimulate immediate skin contraction and continued collagen remodeling over 3-6 months.
Benefits:
- Avoids skin excision scars
- Immediate thermal tightening effect
- Continued improvement over months
- Comprehensive correction without visible scars
Considerations:
- More expensive than standard combination
- Not suitable for severe skin laxity
- Results depend on skin quality and age
4. Periareolar Skin Excision with Combined Approach
What It Is: Sophisticated technique for Grade III gynecomastia with moderate skin redundancy, removing excess skin through a concealed circular incision.
Best Suited Gynecomastia Grades
- Grade III: Noticeable breast fullness with stretched or enlarged areolas and moderate skin laxity.
- Early Grade IV: Sagging breast tissue where lifting the areola and tightening the central skin improves shape.
Ideal Candidates for This Procedure
- Older Male Gynecomastia: Older men with long-standing gynecomastia, stretched or enlarged areolas, and moderate skin laxity who need both lift and volume reduction.
- Post-Weight-Loss Gynecomastia: Men after significant weight loss who have central drooping of the chest and descent of the nipple-areola complex but prefer scars limited around the areola.
- Areolar-Ptosis Gynecomastia: Patients whose primary concern is an enlarged, low, or stretched areola that can be lifted and tightened with a circumareolar (donut) excision.
- Recurrent Gynecomastia with Areolar Deformity: Revision patients with previous surgery and now enlarged or distorted areolas needing reshaping and improved contour.
The Procedure: Begins with Vaser liposuction for fat removal and chest sculpting, followed by gland excision. A doughnut-shaped section of skin is removed around the areola, and outer skin is advanced inward and secured, effectively lifting and tightening the chest while reducing areolar size to masculine proportions (38-42mm).
Benefits:
- Three-layer correction in one operation
- Areolar reduction and repositioning
- Moderate skin tightening
- Single, camouflaged circular scar
Considerations:
- Longer operative time (2.5-3.5 hours)
- Extended compression wear (6 weeks)
- Requires meticulous surgical technique
5. Double-Incision Gynecomastia Procedure
What It Is:
A comprehensive surgical approach used for advanced or severe gynecomastia (Grades III–IV), the Double-Incision Technique removes excess glandular tissue, fat, and redundant skin through two carefully positioned incisions, typically along the inframammary crease. This method provides full access to sculpt and redefine the male chest contour.
Best Suited Gynecomastia Grades
- High Grade III–Grade IV: Marked breast enlargement with significant skin excess and true “male breast ptosis”.
- Cases where the nipple-areola sits low on the chest, similar to a small female breast.
Ideal Candidates for This Procedure
- Post-Bariatric Gynecomastia: Massive weight-loss patients (often after bariatric surgery) with a deflated, hanging male breast and redundant skin extending over the lower chest.
- Extreme Volume Gynecomastia: Patients with heavy breast tissue and low nipple position who require a full chest reshaping rather than just gland removal.
- Scar-Accepting Gynecomastia Candidates: Men who understand that longer, well-placed scars are an acceptable trade-off for achieving a flat, masculine chest contour.
The Procedure:
Two horizontal incisions are placed strategically at the base of the pectoral region. Through these incisions, the surgeon excises glandular tissue and redundant skin, then repositions or grafts the nipple-areolar complex for optimal aesthetic symmetry. Liposuction may also be performed to refine contour and definition.
Benefits:
- Allows full correction of severe cases
- Restores masculine chest contour and proportion
- Permanent results with low recurrence risk
- Enables nipple repositioning for natural symmetry
Considerations:
- Requires board-certified surgeon experienced in complex male chest reconstruction
- Longer recovery period (typically 4–6 weeks)
- Visible but well-concealed scars along natural chest folds
- Temporary changes in nipple sensation possible
6. Skin Resection + Gland Excision (Severe Cases)
What It Is: Comprehensive correction for gyno Grade III-IV with significant skin excess and ptosis.
Best Suited Gynecomastia Grades
- Severe Grade IV: Extreme breast enlargement with major skin redundancy and very low nipple position.
- Complex or revision cases where previous surgery has failed to correct contour or nipple position.
Ideal Candidates for This Procedure
- Extreme Gynecomastia: Patients with the most severe Grade IV gynecomastia, very low nipple position, and massive skin excess that cannot be corrected with limited incisions.
- Post-Bariatric Chest Lift with Gynecomastia: Men after massive weight loss who require both an extensive chest lift and complete gland resection, sometimes with free nipple grafting.
- Complex Revision Gynecomastia: Patients with prior unsuccessful surgeries, irregular scars, or distorted nipple position who need a more aggressive reconstructive approach.
- Chest Feminization Reversal Gynecomastia: Rare cases where the chest has taken on a truly breast-like appearance and requires major skin resection to restore a flat male contour.
- The Procedure: Tailored to degree of skin excess using periareolar, extended periareolar, or free nipple graft techniques. Completely excises glandular tissue, removes redundant skin, and repositions nipple-areola complex.
Benefits:
- Only option for significant skin excess
- Dramatic transformation possible
- Addresses severe ptosis effectively
- Life-changing for massive weight loss patients
Considerations:
- Extended, visible scarring
- Longer recovery (6-8 weeks)
- Most invasive option
| Grade | Characteristics | Recommended Technique(s) |
|---|---|---|
| Grade I (Mild) | Small, localized gland with minimal fat and no skin excess. |
|
| Grade II (Moderate) | Moderate gland and fat; mild areolar fullness; no major skin excess. |
|
| Grade III (Mild Skin Laxity) | Significant glandular tissue with mild skin looseness or early ptosis. |
|
| Grade III (Moderate Skin Laxity) | Significant tissue and moderate excess skin with stretched areola. |
|
| Grade IV (Severe / Post-Weight Loss) | Marked sagging, skin redundancy, and large tissue volume after major weight loss. |
|
Choosing the Right Procedure: Decision Framework

Step 1: Assess Your Grade
Determine your gynecomastia grade (I-IV) based on tissue amount and skin quality.
Step 2: Evaluate Skin Quality
- Excellent elasticity → Standard techniques sufficient
- Mild laxity → Consider Renuvion addition
- Moderate laxity → Periareolar skin excision
- Severe laxity → Full skin resection required
Skin Laxity Decision Algorithm for Grade III
Mild Skin Laxity
Recommended Technique:
VASER + Gland Excision + Renuvion (J-Plasma)
- Age < 50
- Good skin elasticity
- Pinch test < 3 cm
- No areolar enlargement
Moderate Skin Laxity
Recommended Technique:
Periareolar Skin Excision + VASER + Gland Excision
- Visible ptosis
- Areolar stretch > 3 cm
- Requires areolar reduction
Step 3: Consider Your Profile
- Age and healing capacity
- Activity level and athletic goals
- Scar tolerance
- Budget considerations
Step 4: Tissue Composition
- Primarily glandular → Direct excision
- Mixed fat and gland → Combined approach
- Primarily fatty → Liposuction-based technique
For patients who want a general medical overview, the American Society of Plastic Surgeons also provides a concise summary of gynecomastia surgery (male breast reduction).
Risk-Benefit Analysis by Procedure

Lowest Risk Procedures
- Combined Vaser + Gland Excision
- Direct Excision (Subareolar)
Moderate Risk Procedures
- Vaser + Renuvion J-Plasma
- Periareolar Skin Excision
- Double-Incision Gynecomastia Procedure
Higher Complexity Procedures
- Full Skin Resection + Gland Excision
Why Choose GynecomastiaLA in Los Angeles?
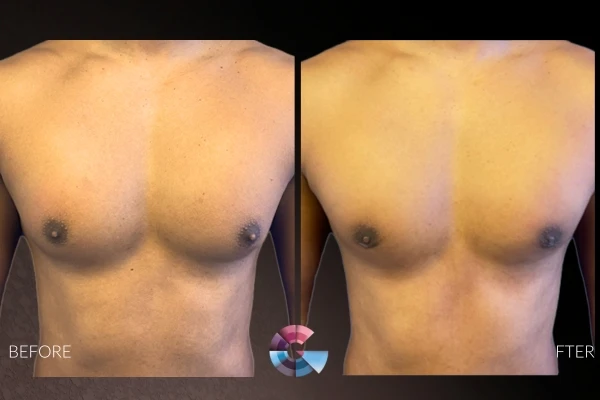
At GynecomastiaLA, patients receive individualized treatment in a discreet, supportive environment tailored for men’s cosmetic needs. Our clinic combines advanced technology with compassionate care to deliver natural, masculine results that restore confidence and body symmetry.
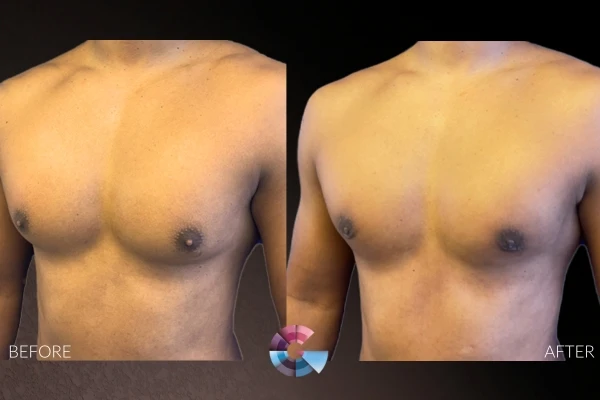
From before-and-after transformations to educational gynecomastia surgery videos, our patients gain a complete understanding of what to expect.
We also offer virtual consultations for those outside Los Angeles, allowing you to discuss your goals directly with Dr. Moein before scheduling your visit.
For personalized guidance, call us today at (310) 896-4043 or contact our office online to begin your transformation journey.
Trust Your Results to Dr. Babak Moein in Los Angeles’ Distinguished Cosmetic Surgeon
With over two decades of surgical experience, Dr. Babak Moein is among Los Angeles’ most respected and double board-certified cosmetic surgeons. Known for his artistry, precision, and consistent patient satisfaction, Dr. Moein has become a trusted name in male chest contouring and advanced gynecomastia correction techniques.
Patients from across California choose Dr. Moein for his commitment to achieving natural, symmetrical, and lasting results, whether through minimally invasive liposuction, VASER-assisted contouring, or comprehensive gland excision.
Schedule your private consultation today to experience expert care from a surgeon recognized for excellence, integrity, and transformative outcomes.

Dr.Babak Moeinolmolki
LA Cosmetic Surgeon Dr. Moein is board-certified by the American Board of General Surgery.