Table of Contents
- Axillary Breast Tissue vs Armpit Fat: Diagnosis, Imaging & Treatment Options
- Axillary Breast Tissue Overview
- History and Physical Examination for Axillary Breast Tissue
- Treatment Options for Accessory Axillary Breast Tissue
- Gynecomastia and Axillary Tissue
- Risk of Malignancy Evaluation and Cancer Screening
- Axillary Breast Tissue vs Armpit Fat Summary
Axillary Breast Tissue vs Armpit Fat: Diagnosis, Imaging & Treatment Options

Differentiating axillary breast tissue, also known as accessory breast tissue or polymastia, from normal fat in the axilla or axillary fat is a frequent and important clinical question raised by surgeons and patients alike. The distinction between these two tissues is relevant to be aware of: axillary breast tissue is hormone-sensitive and may induce cyclic pain and tenderness, and, even though very uncommonly, become a site of the same pathologies within normal breast tissue; in direct comparison, simple axillary fat is merely subcutaneous fat and is typically associated with an individual’s Body habitus or lipohypertrophy. This effort aims to provide a clear and practical comparison of the two tissues, along with an evidence-based approach to evaluating and treating this condition.
Key Differences Between Axillary Breast Tissue and Armpit Fat
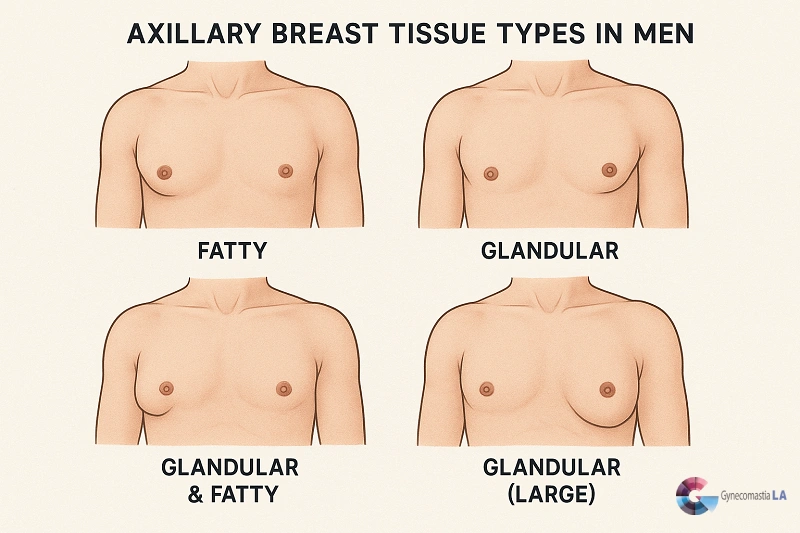
Axillary breast tissue is glandular breast tissue within or in extension into the axilla. It is sometimes denser, nodular, and tender and may change with menstrual or other periods of hormonal change, and may change at puberty, in pregnancy, or with weight alteration.
Armpit fat is the mild subcutaneous fatty tissue which is variable in proportion to total body fat and is usually equally soft in touch, non-nodular and non-tender.
When clinical exam is inconclusive, targeted ultrasound ± mammography clarifies tissue type and rules out lymph nodes, cysts, or suspicious masses.
Management ranges anywhere from observation to liposuction or direct excision; symptomatic or cosmetically problematic ectopic breast tissue is typically resected with gratifying outcomes.
Axillary Breast Tissue Overview
During embryologic development, mammary ridges (“milk lines”) run from the axilla toward the groin. Most of that tissue regresses except at the pectoral region; incomplete regression produces accessory breast tissue anywhere along the line, most commonly in the axilla (including the axillary tail of Spence). That residual tissue can include glandular elements, ducts, and fat, which explains why it behaves differently from plain subcutaneous fat.
History and Physical Examination for Axillary Breast Tissue
Use a focused history and physical exam:
Texture on palpation
Axillary breast tissue: Typically firmer, lobulated or nodular (glandular in character).
Armpit fat: Soft, uniform, compressible adipose tissue.
Tenderness and cyclic change
Accessory breast tissue typically exhibits increased tenderness or detectable swelling during the premenstrual days, in pregnancy, or with fluctuations in hormone levels; in comparison, plain fatty tissue typically does not manifest these cyclic changes.
Mobility and relation to chest wall
The glandular tissue may potentially exhibit a sensation of being rigidly held in place or distinctly separate from the fatty tissue layers above; however, lipomas are usually characterized by their movable nature and sharply defined, well-circumscribed borders. Lymph nodes are usually smaller in size, firmer in consistency, and might be painful or tender if enlarged.
Symmetry & duration
Take into consideration onset (puberty, pregnancy, weight change) and if the bulge is unilateral or bilateral, accessory tissue is typically bilateral but may be unequal.
Ultrasound Imaging and Diagnostic Pathway for Accessory Breast Tissue
If it is uncertain on the exam, if it is a discrete mass, or if it has suspicious features (rapid progression, skin change, fixation, suspicious firmness), ultrasound is the initial imaging modality of choice for the axilla and will aid in differentiation of glandular tissue, lipoma, fluid collection, or lymph node enlargement. Mammography or tomosynthesis is considered when coexisting breast pathology is a consideration or if the imaging reveals a suspicious lesion to be biopsied. Radiologic assessment is relevant because ectopic breast tissue has the same predisposition to benign and malignant change as orthotopic breast tissue.
Treatment Options for Accessory Axillary Breast Tissue

Conservative / observation
- Appropriate when tissue is small, asymptomatic, and imaging is benign. Education about expected hormonal changes and monitoring is usually sufficient.
Liposuction (axillary liposculpture)
- Good for essentially fatty axillary bulges where the issue is subcutaneous fat and not glandular tissue. Minimally invasive, but if glandular tissue is present, then liposuction alone may be correlated to residual hard mound or recurrence.
Direct surgical excision
- Used when the tissue is glandular to relieve pain, restrict shoulder movement, or for cosmetic considerations. Excision provides total extirpation and pathology (excluding malignancy) but usually necessitates a limited incision and discreet scar placement. Surgical outcomes are predictable, with low morbidity rates, in the hands of skilled surgeons.
Combined approach
- If a patient presents with a combination of mixed glandular and fatty tissue, treatment with an integrated approach of gland removal and liposuction typically provides the best cosmetic and functional outcomes for the patient. Furthermore, recent clinical series provide encouraging data to advocate for the safety and efficacy of both nonoperative and surgical treatment methods, particularly when these therapy modality choices are made selectively and appropriately based on the patient’s specific needs.
Gynecomastia and Axillary Tissue
Male patients typically present to the clinic with their concerns about having what they term “armpit lumps.” Further assessment often reveals these lumps to be accessory breast tissue or an extension of glandular breast tissue located laterally and associated with a condition called gynecomastia. Glandular tissue in the breast is prone to enlargement in males in response to several forms of hormonal influences, such as puberty, anabolic steroid usage, and specific drugs.
The differential diagnosis is crucial for distinguishing true gynecomastia from localized fatty pseudogynecomastia and accessory tissue. This is because it determines the correct management plan, which includes a workup to identify the underlying hormonal cause of these lumps, an imaging study, and consideration of tissue-specific removal when it is symptomatic or cosmetically unacceptable.
Risk of Malignancy Evaluation and Cancer Screening
Accessory breast tissue has the same propensity to develop the same pathologies as ordinary breast tissue and may develop carcinoma. Cancer in accessory tissue is rare but has been reported; hence, any questionable mass, scleral fixation, skin retraction, or questionable imaging necessitates biopsy and oncologic consultation. Screening removal of symptomatic accessory tissue offers both symptomatic relief and histologic diagnosis.
Preoperative Planning & Patient Counseling
Plan imaging in advance (ultrasound ± mammogram) and discuss the likely tissue composition and options (liposuction vs excision vs combined).
Set the patient’s expectations about scars, shaping, and the possibility of post-operative stiffness if glandular tissue is retained.
Discuss pathology: tissue from an otherwise complete resection should be sent for histology if an atypical feature is present or if the patient requests it.
Rehabilitation: Early post-operative mobilization of the shoulder decreases stiffness; wound care and activity schedule counseling are also provided.
Clinical Decision Algorithm to Treat Axillary Tissue in Clinical Practice
If examination is suggestive of fatty axillary fullness → weight loss consideration or trial of conservative management or liposuction; if examination is suggestive of nodular, hormonally alterable, or tender tissue → ultrasound evaluation and plan coordinated combined excision (or combined excision + liposuction) with pathology.
Axillary Breast Tissue vs Armpit Fat Summary
Accurately distinguishing axillary breast tissue vs armpit fat guides safe, effective treatment. For patients bothered by axillary bulges, cyclic tenderness, or cosmetic concerns, a focused clinical examination and ultrasound can clarify the situation, and treatment choices (such as liposuction, removal, or combined procedures) can be customized to achieve superb results. If an evaluation, imaging conference, or surgical consult would be beneficial to a patient, or if you’d like an opinion on a patient presenting with these characteristics or symptoms, our Gynecomastia LA physicians offer specialized evaluations and custom surgical plans. Schedule an appointment at here or call our office to arrange an appointment.

Dr.Babak Moeinolmolki
LA Cosmetic Surgeon Dr. Moein is board-certified by the American Board of General Surgery.