Etiology of Grade 2 Gynecomastia: ROUNDED CHEST
Overview
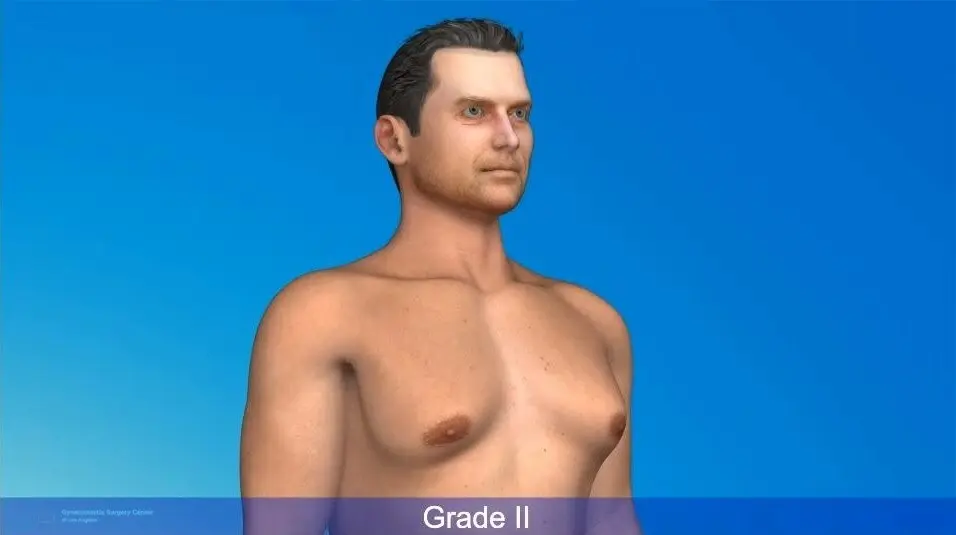
Grade 2 gynecomastia is marked by moderate breast tissue growth with a small amount of excess skin. This separates it from other degrees where there is more extra skin. The chest fold has a tight, rounded shape, giving the chest a fuller, more prominent contour.
Different surgical treatments may help, including endoscope-assisted and direct excision methods. This type is most commonly seen in individuals aged 15 to 40, often frustrated young adults seeking a more masculine chest profile.
Gynecomastia, the enlargement of male breast tissue, is a condition that can significantly impact self-esteem and body image. Among its various classifications, Grade 2 gynecomastia presents unique challenges and requires a nuanced understanding for effective management.
Understanding the complexities of Grade 2 gynecomastia involves exploring multiple facets, including hormonal imbalances, genetic predispositions, and environmental factors.
Gynecomastia Surgery for a Sculpted, Masculine Chest

Understanding Grade 2 Gynecomastia
Grade 2 gynecomastia involves moderate breast enlargement that may be associated with exxtension into the armpit. Contour changes are typically more dramatic with fullness extending into the armpit making it more noticeable even under loose clothing. Treatment for grade 2 gynecomastia is unique and involves three separate approaches.
Surgical Options:
- Liposuction: Removes excess fatty tissue over both the chest and armpit region.
- Direct Excision: Targets glandular tissue
Choosing a Professional Gynecomastia Surgeon and Specialized Center

What Causes Grade 2 Gynecomastia?
Hormonal Imbalances
Hormonal imbalances are a key cause of gynecomastia. Higher estrogen, lower androgen levels, receptor defects, or increased tissue sensitivity to estrogen can all contribute. These imbalances can happen during various life stages of men, like in puberty. True gynecomastia often stems from such hormone-related issues. Medical treatment aims to balance estrogen and androgen levels, possibly through medications that block estrogen or increase androgens. If gynecomastia lasts beyond a year, it becomes fibrous, making medical treatments less effective.
Genetic Factors
The development of gynecomastia suggests possible genetic predispositions. Conditions like hypogonadism, which can be hereditary, might lead to the condition. The hormone balance, particularly the estrogen-to-testosterone ratio, plays a big role. Some tumors that affect hormone glands may also have genetic links, affecting testosterone levels and causing gynecomastia. A genetic tendency towards decreased testosterone in older age can further shift hormone balance, increasing the risk of developing gynecomastia.
Environmental Influences
Environmental factors also play a role in gynecomastia. Changes in testosterone levels or the use of certain medications in older men can trigger it. Obesity, too, can impact hormone levels, thus influencing breast tissue growth. Neonatal gynecomastia occurs due to maternal estrogen exposure, affecting 60%-90% of newborn males. Adolescence is another phase where hormone shifts happen, partly due to environmental impacts on adrenal and hormone functions.
Pathogenesis of Grade 2 Gynecomastia

Grade 2 gynecomastia is a condition marked by moderate breast enlargement with some extra skin. This can be quite noticeable, even under looser clothing. Simons classification system helps evaluate this by looking at how much breast tissue has grown and the skin's appearance. For cases like this, surgery is often needed. The options include liposuction or vaser, direct excision, or both. These aim to remove the excess tissue and correct the skin. Many patients find their quality of life improves after surgery. They often report feeling better about themselves in assessments like the RSES and SF-36v2. The outcome of surgery can vary, but results are often seen as very good, good, or average depending on certain criteria.
Mechanisms of Tissue Growth
Gynecomastia happens mainly due to hormonal imbalances. Estrogen levels go up, while testosterone levels fall. For teenage boys, it can be a temporary issue due to hormones. Estrogen can suppress luteinizing hormone, which affects how much testosterone is made, increasing breast tissue. Sometimes, tumors in areas like the adrenal glands, pituitary glands, or lungs cause this imbalance by altering hormone levels. Increased sensitivity to normal estrogen levels can also be a problem, leading to tissue growth even when androgen levels seem normal.
Role of Adipose Tissue
Adipose tissue, or body fat, plays a key role in gynecomastia. It contains enzymes that convert androgens into estrogens. This can disrupt hormone balance. Gynecomastia is often more common in obese adolescents. Studies find that 51% of those with gynecomastia are obese. There's a clear link between a higher BMI and increased breast tissue in males. Obese males often have high estrogen and low testosterone levels. Reducing body weight can help, as weight loss improves testosterone levels. This shows how crucial it is to manage body fat to maintain hormonal balance and potentially reduce gynecomastia.
In summary, understanding and managing gynecomastia involves recognizing its hormonal and physiological roots. Through surgical and lifestyle interventions, many can achieve better outcomes and quality of life.
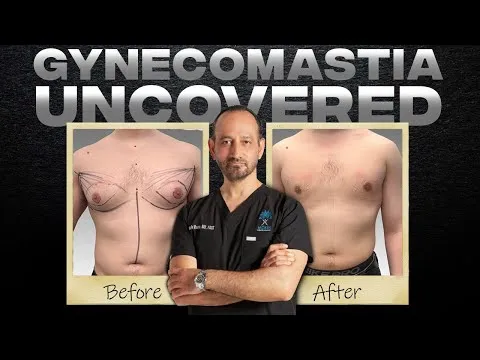
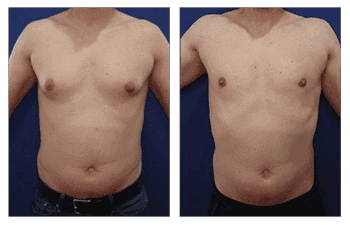
Before and After Grade 2 Gynecomastia



Clinical Features of Grade 2 Gynecomastia
Grade 2 gynecomastia features moderate enlargement of the breasts with some extra skin around the areola. This level of growth is noticeable, even under loose clothing. Causes often include hormonal imbalances, certain medications, weight gain, and long-term anabolic steroid use. The result can be a breast appearance similar to that of a female, with folds of redundant skin. Surgical options like liposuction and direct excision of the gland which is combined with tightening the overlying skin of the chest.
Physical Examination Findings
A thorough physical exam helps diagnose grade 2 gynecomastia. It includes a close look at the breast tissue for any swelling, nipple discharge, or skin changes. The testicular exam is important, too, especially for older men, as it helps rule out testicular tumors and male breast cancer. In addition to the breast exam, doctors should check the abdominal and urological systems. This will exclude other conditions like testicular tumors or liver disease. If the exam suggests a benign issue, a breast ultrasound is a good start. Otherwise, more detailed tests like a core needle biopsy may be needed. In preparation for surgery, surgeons should review symptoms' duration, family history of breast cancer, and any nipple discharge.
Symptoms and Patient Complaints
The main symptom of grade 2 gynecomastia is self-consciousness about breast appearance. This can lead to psychological stress. Patients may also report tenderness or pain in the enlarged breast tissue. Symptoms often include enlargement and lumps. Most treatment requests are due to appearance concerns rather than physical pain. Patients with a normal body type usually report higher satisfaction with surgical outcomes.
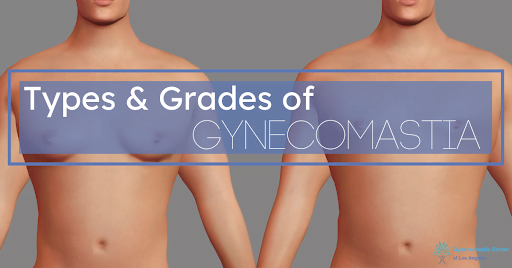
Differentiating Grade 2 from Other Grades
Grade 2 gynecomastia involves moderate breast enlargement that extends into the armpit region. This separates it from Grade I, which shows less aggressive growth limited to the chest region. According to Dr. Moein's grading system, Grade 2 sits between moderate and more severe types. The condition is visible even in loose clothes, urging many patients to consider surgery.
Comparison with Grade 1 and Grade 3
Grade 2 gynecomastia falls between Grade I and Grade 3 in severity. In Grade I, there is a minor enlargement of breast tissue around the areola without significant skin excess. Surgical management is often less invasive, involving small gland excision minor liposuction over the chest only.
For Grade 3, there is a marked enlargement, resembling a female breast that extends into the armpit region. This grade requires surgical excision of the gland but also more generous liposuction that extends into the armpit region. Such extensive procedures can impact post-operative recovery and patient satisfaction.
Grade 2 involves moderate to severe enlargement with involvement of the axilla. Treatment often balances between less invasive techniques of Grade I and the more comprehensive surgical approaches needed for Grade 3. Patients with Grade 2 may require more intervention than those with Grade 2, but less than those with Grade 3.
Management options vary based on the specific case, but severe grades like III often need more invasive surgical approaches compared to the milder Grade I. As the severity increases, the effectiveness of non-surgical, medical therapies declines. A tailored treatment plan ensures the best correction of gynecomastia based on individual needs.
Risk Factors for Developing Grade 2 Gynecomastia

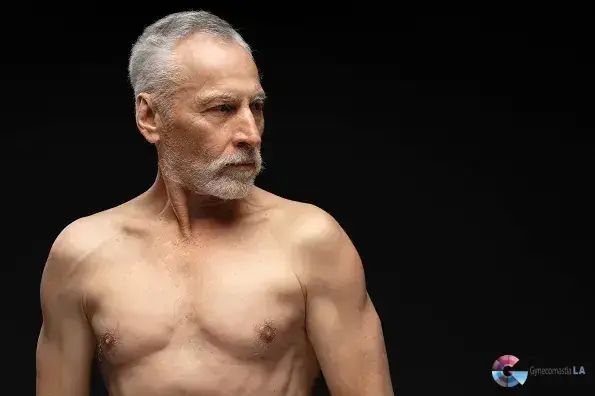
Grade 2 gynecomastia is marked by moderate breast enlargement with minor skin excess that occurs in older patients. This presents unique challenges in management, especially concerning skin redundancy and potential scarring. Successful treatment often requires careful surgical techniques to address these issues.
Obesity and Metabolic Factors
Obesity is a key risk factor for gynecomastia. A study found that 51% of patients with gynecomastia are obese. This condition can lead to hormonal imbalances, where the level of estrogen increases compared to testosterone.
This hormonal shift encourages the growth of glandular tissue in the breasts. Other health conditions like hypogonadism and liver disease can also cause gynecomastia. Interestingly, research studies usually avoid patients with morbid obesity, highlighting its significant impact on the condition.
Treatments for gynecomastia aim to restore hormonal balance. Common medications include Raloxifene, Danazol, and Anastrozole. Their effectiveness can vary, especially in teens. Estrogen increases glandular tissue and lowers testosterone by blocking luteinizing hormone, which is essential for testosterone production. Some medications, such as estrogens and certain diuretics, may lead to gynecomastia. Testosterone replacement can sometimes help, particularly in hypogonadal patients, but there is a risk of worsening the condition if testosterone converts to estrogen. Testolactone, which blocks estrogen production, has shown promise in treating early-stage pubertal gynecomastia.
Age and Physiological Changes
Gynecomastia can appear in infancy due to maternal estrogen and usually disappears within weeks. Another peak period is during puberty (ages 10 to 17), when hormonal shifts can cause a temporary imbalance between estradiol and testosterone, often resolving by age 17. In older adults (ages 50 to 80), declining testosterone levels and medication side effects can trigger gynecomastia. These age-related peaks infancy, puberty, and older adulthood comprise 75% of idiopathic gynecomastia cases.
Overall, understanding these risk factors allows for better management strategies tailored to individual needs.
Diagnosis of Grade 2 Gynecomastia in Los Angeles, CA
Grade 2 gynecomastia is notable for moderate breast tissue enlargement that may extend into the armpit. This classification is part of the Moein grading system, which helps assess severity based on breast size and skin redundancy. Recognizing Grade 2 is crucial for choosing the most suitable surgical techniques. Surgical management usually involves removing glandular tissue and liposuction of the chest and armpit region and occasional treatment of skin excess, aiming to minimize scarring. Patients with this condition often face psychological challenges due to visible chest changes, prompting many to seek surgical correction.
Clinical Assessment
A detailed clinical assessment is vital for diagnosing gynecomastia. This involves examining the breast for swelling, skin changes, and nipple discharge. It is also essential to check the axillary and regional lymph nodes. A testicular exam is crucial, as gynecomastia can be linked to testicular tumors. Differentiating gynecomastia from male breast cancer in older men is a key part of the assessment. While the use of hematologic tests is debated, many centers advocate screening for adults. A proper diagnosis also includes a history review, focusing on medications and drugs.
Imaging Techniques
Breast ultrasound is the first choice for imaging in gynecomastia due to its affordability and high accuracy. It has no X-ray exposure. If the ultrasound shows abnormalities, further tests like mammograms or MRIs might be needed. The imaging process starts with a physical exam and breast ultrasound to exclude other diagnoses. Patients with benign findings may only need an ultrasound, but concerning results require more tests, such as core needle biopsy. Surgical candidates undergo lab work and imaging to explore causes, including hormone levels.
Treatment Options for Grade 2 Gynecomastia
Grade 2 gynecomastia can be addressed through both non-surgical and surgical options. Treatments should be chosen based on the patient’s needs and the condition's persistence. Below are the different methods used to manage this condition effectively.
Pharmacological Interventions
Pharmacological treatments aim to balance hormones, which often cause gynecomastia. Medications like Raloxifene, Danazol, and Anastrozole are commonly used. These drugs may help reduce breast tissue but have varied effectiveness. It's important to discuss potential side effects with a medical provider. For many, medication serves as the first step before considering surgery.
Surgical Interventions
Surgical treatment is suggested when gynecomastia persists despite medical therapies. Techniques vary, allowing for tailored approaches based on the patient. One advanced method includes Renuvion skin tightening. Satisfaction rates for surgical procedures are high, often exceeding 84.5%. Choices between liposuction and subcutaneous mastectomy depend on factors like age and body type. The aim is optimal recovery with excellent results.
Direct Gland Excision
Direct gland excision is accomplished using a small incision located on the undersurface of the areola. Through this port hole, the gland is directly observed and resected. Removal of the gland is an artform, as overresection may result in a crater nipple deformity, but typically patients should expect removal of more generous specimens when compared to grade 1 gynecomastia.
Liposuction of the Chest
Liposuction of the chest and armpit region is a critical component for the treatment of more moderately sized chest contour. Liposuction is performed following gland excision to ensure a smooth and flat chest contour. This step involves use of sleek cannulas that are strategically inserted to remove prominence of the soft tissues throughout the chest and armpit region.
Renuvion Skin Tightening
Renuvion skin tightening has become the mainstay for the reduction of skin laxity that is often apparent in older clients. Renuvion uses a combination of Helium plasma technology and radiofrequency energies to thermally treat the collagen in the underlying skin and soft tissues. The transfer of heat to the collagen results in a shrink wrap effect which tightens the skin of both the chest and armpit region.
Evaluating Gynecomstia Treatment Efficacy in Los Angeles, CA
Gynecomastia, the enlargement of male breast tissue, can be distressing. Tamoxifen, an antiestrogen medication, is a common treatment option. It blocks estrogen's effects on breast tissue, often effectively treating idiopathic and pubertal gynecomastia. Although studies show promise, more robust research, like randomized controlled trials, is needed to confirm these results.
Surgical approaches also play a key role in managing gynecomastia. The Simon classification system helps in evaluating surgical outcomes based on the severity of the condition. Enhanced liposuction, paired with pull-through and bottom-up techniques, has shown positive results, especially for grade I and II gynecomastia. These methods reduce scarring and increase patient satisfaction.
Success Rates of Various Gynecomastia Treatments
Recovery times are also shortened with these methods. Patients typically stay in the hospital for about 1.2 days after a combination of liposuction and subcutaneous mastectomy. For non-obese male adolescents with persistent pubertal gynecomastia, surgical management is advisable. It effectively reduces breast pain and emotional distress.
When it comes to treating gynecomastia, different methods show varying success rates. Enhanced liposuction combined with pull-through and bottom-up techniques in grade I and II cases results in high patient satisfaction, averaging 4.68 out of 5 points. A review indicated this combined approach, including surgical excision and liposuction, leads to fewer complications compared to surgical excision alone. The complication rate is 11.76% compared to 30.64% for surgery alone.
Patient Satisfaction and Quality of Life
Gynecomastia treatment often leads to high patient satisfaction. Studies show mixed levels of satisfaction, but many patients report being pleased post-surgery. For example, 70% of patients rated their results as ‘excellent’ during the second follow-up. On a 5-point scale, surgical intervention scores an average of 4.4, highlighting general satisfaction with both comfort and appearance.
Furthermore, gynecomastia treatments significantly improve life quality. Patients report better outcomes in terms of physical comfort and self-esteem. This indicates that surgical intervention plays a vital role in enhancing overall well-being for those undergoing gynecomastia treatment.
Challenges in Managing Grade II Gynecomastia
Grade II gynecomastia presents numerous challenges. It involves significant breast enlargement with excess skin. This condition often results from hormonal imbalances or weight changes. Surgical intervention is typically necessary, as it seldom resolves on its own.
Several surgical techniques have been developed to treat grade IIB gynecomastia. These include methods that combine liposuction and glandular tissue removal. The excess skin can complicate surgical management. This often requires additional procedures for skin removal and contouring.
Techniques, like the double donut approach, aim to minimize scarring. They also allow for effective breast tissue removal. Here is a summary of key surgical approaches: Surgical success depends on addressing both tissue and skin concerns simultaneously.
Psychological Impact on Patients
Gynecomastia can cause significant psychological effects, especially in adolescents. This condition often leads to embarrassment and distress. Many feel insecure about their appearance, which can deeply influence their self-esteem.
Surgical treatment has shown improvements in social and emotional well-being. Men who undergo surgery often experience enhanced social activity and acceptance. High satisfaction levels are reported, relating to comfort and appearance.
For some patients, gynecomastia's psychological strain is severe. This may require counseling, alongside medical or surgical intervention. Here are the common psychological impacts:
- Embarrassment and emotional distress
- Insecurity about physique
- Impact on self-esteem
- Improved social and emotional comfort post-surgery
Overall, addressing both physical and emotional aspects is crucial for holistic treatment.